- What cancers are caused by high-risk HPV?
- High-risk HPV related issues
- Myths surrounding HPV
- How can I reduce my risk?
- The HPV Vaccine in Ireland
What is HPV?
HPV stands for ‘human papillomavirus’, which is a group of more than 100 viruses.
Around 40 types of HPV can infect the genital tract of both men and women, and over 75% of people in Ireland dont really understand what HPV is. HPV virus strains can be catagoriesed into two types, low risk and high risk. Some of the low risk types (e.g. HPV 6 and 11,) can go unnoticed or cause genital warts, where as 14 high risk HPV strains are known to be cancer causing. 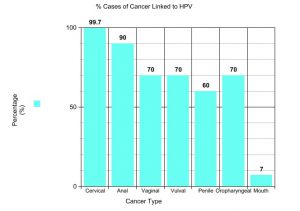 Like other viral infections, most cases of HPV will be cleared by the body’s own immune system. However, a small percentage of people do not clear the infection, which can remain dormant in their bodies sometimes for many years. We don’t know why some people’s immune systems clear the infection and some people’s do not. For most, 90% of new infections clear within 2 years. 13 high risk HPV types have been identified. People infected with ‘high risk’ HPV types that go untreated are more likely to go on to develop cancer.
Like other viral infections, most cases of HPV will be cleared by the body’s own immune system. However, a small percentage of people do not clear the infection, which can remain dormant in their bodies sometimes for many years. We don’t know why some people’s immune systems clear the infection and some people’s do not. For most, 90% of new infections clear within 2 years. 13 high risk HPV types have been identified. People infected with ‘high risk’ HPV types that go untreated are more likely to go on to develop cancer.
The HPV virus is very common; around eight out of ten people (80%) will be infected with the virus at some point in their lives. Research shows that almost every sexually active adult will have at one point been in contact with HPV.
The majority of HPV infections do not cause any symptoms. This is known as being asymptomatic.
High risk HPV 16, 18, 31, 33, 35, 45, 51, 52, and 56, untreated have been linked to cervical, oropharynx, anus, vagina, vulva and penis cancers. The oropharynx is the name given to the part of the throat at the back of the mouth. It includes the back third of the tongue, the soft palate, the side and back walls of the throat, and the tonsils.
It has also been shown that 99 % of all cervical cancers can be traced back to HPV. The virus has also been shown to cause 1 in 20 cases of cancer worldwide.
Click here to view a HPV Aware infographicHow is the HPV virus spread?
HPV is spread by close ‘skin to skin’ contact during any kind of sexual activity. This includes vaginal, anal and oral sex or genital contact with a person that has HPV. Condoms will reduces, but not eliminate the risk of contracting HPV as the virus can affect areas not covered by a condom.
What cancers are caused by the ‘High risk’ HPV virus?
HPV is reported to be responsible for approximately 1 in every 20 cases of cancer across the world. In Ireland, an average of 406 cancers can be linked to an HPV infection in both women and men every year.
High risk HPV viruses can cause a range of pre-cancerous lesions – abnormal cells – in both men and women.
High risk HPV virus causes:
- Almost all cases of cervical cancers
-

HSE list of frequently asked questions 9 out of 10 vulval cancers (the area around the opening of the vagina)
- 7 out of 10 vaginal cancers
- 9 out of 10 HPV-related anal cancers
- 9 out of 10 cases of genital warts (Genital warts are not cancer and do not cause cancer but are very uncomfortable and can come back)
The HPV virus can also cause some cancers of the head and neck.
Download a leaflet of frequently asked questions published by the HSE here and learn all you need to know about how HPV can effect you.
Myths surrounding HPV
When it comes to HPV, there is a lack or awareness, or simply a spread of misinformation about what HPV actually is, and how it can be prevented. The list below are some of the most common myths surrounding HPV.
- HPV is not common??
After being diagnosed, some people feel like they are the only person they know with HPV. It’s easy to understand why so many people feel this way. Public awareness of the virus is extremely low with only 25% of the population actually understanding what HPV is. In reality, around eight out of ten people (80%) will be infected with the virus at some point in their lives
- Women in a gay relationship can’t catch the virus and don’t need a smear?? Untrue
HPV can be passed through other forms of skin-to-skin contact as well as penile-vaginal sex or anal sex.
- Older women can’t get cervical cancer or contract HPV infection?? Untrue
It is most frequently diagnosed in women between the ages of 35 and 44. It rarely affects women under age 20, and more than 15 % of diagnoses are made in women older than 65. The average age of diagnosis in Ireland is 46.
- Genital warts cause cancer? Not TRUE
The truth is that the growths we call genital warts are almost always benign. In the vast majority of cases, they do not lead to cancer, turn into cancer, or indicate that a person will at some point develop cancer.
- Condoms prevent the risk of contracting HPV ??
Used correctly, condoms are very effective against STIs that are spread through bodily fluids. However, they are likely to be less protective against STIs that spread through skin-to-skin contact, such as HPV and herpes. The reason is simply that condoms do not cover the entire genital area of either sex. They leave the vulva, anus, perineal area, base of the penis, and scrotum uncovered, and contact between these areas can transmit HPV.
How can I reduce the risk of having a persistent HPV infection?
Individuals can reduce their risk of getting an HPV infection by:
- Not smoking – Smoking stops the bodies immune system from working properly, leaving a person more likely to develop HPV infections. A study done by the International Agency for Research on Cancer (IARC) showed that cervical squamous cell carcinoma (SCC) risk is 46% higher in current smokers versus never-smokers. Cervical SCC (invasive or in situ) risk increases with number of cigarettes smoked per day.
- Changes in sexual behaviour – Reducing the number of sexual partners and the frequency of new partners can also reduce the risk. HPV can also be contracted in long-term relationship as in a one-night stand.
- Wearing a condom – Condoms can help reduce the risk of being infected with HPV but it will not completely eradicate the risk as HPV lives on the skin in and around the whole genital area
- Leading a healthy lifestyle – Keeping your immune system (bodys natural defence against disease and infection) strong is important.
- Getting HPV vaccinated –HPV vaccine protects against the HPV virus which can cause cancer and genital warts in both women and men. The HPV vaccine Gardasil 9 protects against the types of HPV that cause 9 out of 10 cervical cancers.The HPV vaccine has greatly reduced cases of pre-cancers of the cervix in young women in many countries including Australia, Sweden, the US and the UK. In countries where the HPV vaccine is used, the number of cases of genital warts has decreased dramatically in both young women and men. For more about the HPV vaccine, visit our page or click here for the information from the HSE.
However it is important to note that the HPV vaccine doesn’t protect against all types of HPV. Cervical screening is another effective way to reduce the risk of developing cervical cancer.
The HPV vaccine in Ireland
Awareness about what HPV is and how common it is very low in Ireland. Research done by MSD shows that 53% of parents dont worry about their sons contracting HPV, while 62% of the people think that HPV is a rare condition. Thankfully, vaccines are now available which give more than 99% protection against infection from high risk HPV types.
National HPV Immunisation Programme
Since September 2019, the National Immunisation Programme has offered the HPV vaccine (Gardasil 9) to first year boys and girls across Ireland. This vaccine helps to protect against 90% of cancer causing HPV virus strains. For more information about the HPV vaccine, visit HPV.ie
Visit HPV Information Materials for more information about the school programme and how you can protect your child.
For more about the vaccine, visit The HPV Vaccine page on this website.
For support and information for those affected by Gynaecological cancer, visit ThisIsGo.ie by clicking here.
HPV vaccine for older boys and girls
HPV vaccine catch-up programme
The Laura Brennan Catch-up programme which was launched in December 2022 has now officially come to an end. This was a free HPV vaccination programme for people who missed the vaccine in first year in secondary school. It was free for females in 2nd to 6th year of secondary school and up to the age of 25 and for all males up to their 22nd birthday (Since August 2023).
Right now, from this month going forward, it is just free for 1st year boys and girls in secondary school.
If any person began their vaccination course with the Laura Brennan FREE HPV Catch-up Vaccination Programme and required 3 vaccine doses due to being immunocompromised then they should complete their course in line with NIAC timing recommendations. This offer will be delivered by the HSE vaccination teams.

